What Are The Factors You Need To Consider When Coding For Wound Repair?

Office iii: Scour the documentation for three key details to correctly code for wound repair.
Accurately coding dermatological procedures tin be tricky. Information technology is imperative that medical coders empathise the anatomy of the skin and tin can extract specific information from the clinical documentation. We've spent the last two months reviewing the codes and guidelines for damaged pare treatment services by means of skin tag removal, shaving, and lesion excision. In this third and final installment, we'll discuss coding for wound repair (closure) procedures using CPT® codes 12001-13160.
Proper code choice when reporting a wound repair procedure requires examining the clinical documentation to determine three things:
- Layers involved (complexity of the repair: simple, intermediate, or circuitous);
- Location of the closed wound; and
- Length, in centimeters, of the closed wound
Each of these variables is specified in the CPT® repair codes. The repair can consist of sutures, staples, or tissue adhesive (for case, Dermabond), either singly or in combination with each other, or with adhesive strips. Wound closure using adhesive strips as the simply repair material should be reported using the advisable evaluation and management (E/Thou) code. Wounds repaired solely with Dermabond or other tissue adhesive are reported to Medicare with HCPCS Level II code G0168 Wound closure utilizing tissue adhesive(s) just. Commercial carriers permit unproblematic repair codes (12001-12018). Permit'due south examine the three key elements that are crucial in determining the correct wound repair lawmaking.
1. Determine Repair Complexity
Showtime, determine the complexity of the repair. Repair codes are divided into three categories:
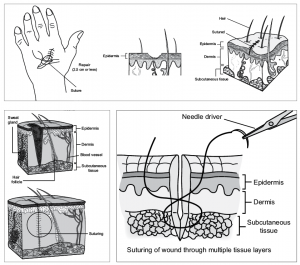
- Simple repairs (12001-12021) are for superficial wounds with partial- or full-thickness damage to the skin (epidermis/dermis) and possibly the subcutaneous tissue. Deeper structures are not involved, and these repairs require merely a simple 1-layer closure. These straightforward repairs involve the skin; deeper layers, such as muscle, remain unaffected. Anesthesia and chemical or electrocauterization of wounds are included.
- Intermediate repairs (12031-12057) involve a layered closure of ane or more of the deeper layers of the subcutis and superficial (non-muscle) fascia, in addition to the skin (epidermal and dermal) closure. Wounds necessitating an intermediate repair are generally deeper or gaping, requiring suture placement inside the wound to approximate tissue layers below the skin. Per CPT®, "Unmarried-layer closure of heavily contaminated wounds that have required extensive cleaning or removal of particulate matter also constitutes intermediate repair." When searching the documentation for clues regarding complication, statements such equally "layered closure," "extensive cleaning," and/or "removal of debris" betoken an intermediate repair. Lack of these details or mention of a "single-layer closure" suggests a simple repair.
- Complex repairs (13100-13160) care for deeper, more than extensive wounds that require more than a layered closure such every bit debridement, extensive undermining, stents, scar revision, or retention sutures. Complex repairs include wounds that necessitate the creation of a express defect for repairs or the debridement of complicated avulsions or lacerations. Documentation should detail extensive reconstructive repair necessitating procedures more than involved than cleansing and suturing at one or more levels.
2. Identify Location Subcategory
After you take determined the complexity of the repair, the next step is to identify the body site(due south) being repaired. Within each level of repair, wounds are classified according to anatomic location. Note that these categories are not identical for each level of repair.
- Simple repairs:
- Scalp, neck, axillae, external ballocks, trunk, and/or extremities (including easily and feet) (12001-12007)
- Face, ears, eyelids, nose, lips, and/or mucous membranes (12011-12015)
- Intermediate repairs:
- Scalp, axillae, torso, and/or extremities (excluding hands and anxiety) (12031-12037)
- Neck, hands, anxiety, and/or external ballocks (12041-12047)
- Confront, ears, eyelids, nose, lips, and/or mucous membranes (12051-12057)
- Complex repairs:
- Trunk (13100-+13102)
- Scalp, arms, and/or legs (13120-+13122)
- Brow, cheeks, chin, rima oris, neck, axillae, genitalia, hands, and/or feet (13131-+13133)
- Eyelids, nose, ears, and/or lips (13151-+13153)
3. Effigy Wound Length
Last lawmaking selection is based on the size of the repair. The length of the wound repaired must exist measured and recorded in centimeters, whether curved, angular, or stellate. If the wound measurements are documented in inches or millimeters, instead of centimeters, convert the measurements to centimeters before selecting the appropriate lawmaking.
Additional Considerations
Coding Multiple Repairs
Oft, the doc repairs several wounds in a unmarried session. When multiple wounds are repaired, check if whatsoever repairs of the same nomenclature (simple, intermediate, complex) are grouped to the same anatomic area. If so, per CPT® coding guidelines, the lengths of the wounds repaired should be added together and reported with a unmarried, cumulative code. Do Non combine wounds of unlike complexity or those that fall within separate anatomical location groupings.
When reporting wounds of differing severity and/or location, claim the well-nigh all-encompassing code every bit the master service and append modifier 59 Distinct procedural service to subsequent repair codes. Multiple procedure reductions will use for the 2d and subsequent procedures, except for those reported using an improver code.
To Bundle or Non to Bundle
Wound repair is often performed with other related procedures. Some of these related procedures can exist separately reported, while others can't or depend on specific circumstances. Here'southward a breakdown of how to determine when separate reporting is warranted.
Never reported separately with wound repair:
- Whatever service considered part of the global surgical package, such as topical anesthesia, writing orders, and immediate/typical postoperative care. For more details, see the Surgical Package Definition in the CPT® Surgery Guidelines. Be aware that Medicare defines the surgical package differently; for more information, refer to the Medicare Claims Processing Transmission.
- Chemic or electrocauterization.
- Uncomplicated ligation of vessels in an open wound.
- Simple exploration of nerves, blood vessels, or tendons in an open up wound. More extensive exploration may be reported separately, as explained below.
- For circuitous wound repairs, do non study the creation of a limited defect or the debridement of complicated lacerations or avulsions, as that is considered necessary preparation.
Sometimes reported separately with wound repair:
- Decontamination and/or debridement services provided in conjunction with wound repairs are not coded separately unless the documentation specifies that gross contamination required prolonged cleansing, that appreciable amounts of devitalized or contaminated tissue were removed, or when debridement is carried out separately without immediate main closure.
- Lesion excision includes simple repairs, but repairs using intermediate or circuitous closure should be reported separately.
E'er reported separately with wound repair:
- Excisional preparation of a wound bed or debridement of an open up fracture or dislocation when performed with a circuitous repair.
- Circuitous repair of fretfulness, blood vessels, and tendons.
- "If the wound requires enlargement, extension of autopsy (to decide penetration), debridement, removal of strange torso(s), ligation or coagulation of small subcutaneous and/or muscular blood vessel(south) of the subcutaneous tissue, muscle fascia, and/or muscle, not requiring thoracotomy or laparotomy, use codes 20100-20103, every bit advisable," per CPT®.
Avoid common coding mistakes by remembering the three fundamental components for coding wound repair correctly: complication, location, and length. Detailed documentation is critical in determining these details, which ensures coding precision and proper payment for services rendered.
https://world wide web.aapc.com/blog/49304-complexities-of-skin-procedure-coding/
- Author
- Recent Posts
![]()
Source: https://www.aapc.com/blog/49780-wound-repair-coding-in-3-easy-steps/
Posted by: bolesdound1945.blogspot.com


0 Response to "What Are The Factors You Need To Consider When Coding For Wound Repair?"
Post a Comment